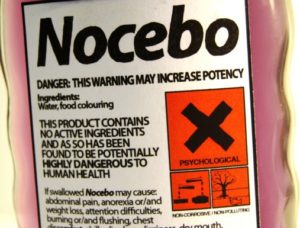
As practitioners become a little more ‘open’ about their use of placebos, it’s time now to discuss the ethics of such use. From Glackin’s abstract:
It is widely supposed that the prescription of placebo treatments to patients for therapeutic purposes is ethically problematic on the grounds that the patient cannot give informed consent to the treatment, and is therefore deceived by the physician. This claim, I argue, rests on two confusions: one concerning the meaning of ‘informed consent’ and its relation to the information available to the patient, and another concerning the relation of body and mind. Taken together, these errors lead naturally to the conclusion that the prescription of placebos to unwitting patients is unethical. Once they are dispelled, I argue, we can see that providing ‘full’ information against a background of metaphysical confusion may make a patient less informed and that the ‘therapeutic’ goal of relieving the patient of such confusions is properly the duty of the philosopher rather than the physician. Therapeutic placebos therefore do not violate the patient’s informed consent or the ethical duties of the doctor.
The whole paper can be found here. It seems the article has stirred up something of a hornet’s nest among ‘psychopharmacologists’ – see the recommendations listed at the foot of the website.