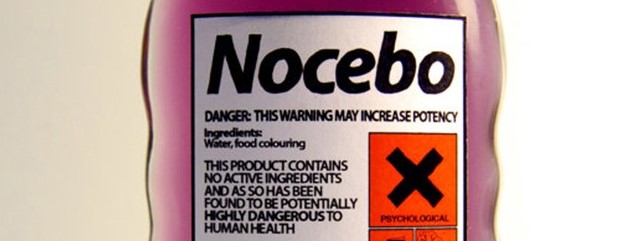
Recent studies show that users’ anticipations and beliefs about a technology can significantly influence their experiences, behaviours, and even cognitive processing – independent of the system’s actual functionality.
In one study (Villa et al. 2023) participants exhibited a placebo effect through increased risk-taking after being exposed to the sham brain-computer interface. This suggests their mere belief in cognitive augmentation led to changes in risk-taking behavior, even though no actual enhancement took place. Additionally, brain imaging (EEG) data revealed differences in how participants processed information, particularly related to losses, under the placebo condition compared to control. This implies the placebo effect can significantly influence not just behavioural outputs but also the underlying neural processes involved in cognition.
More information about these studies is available here.