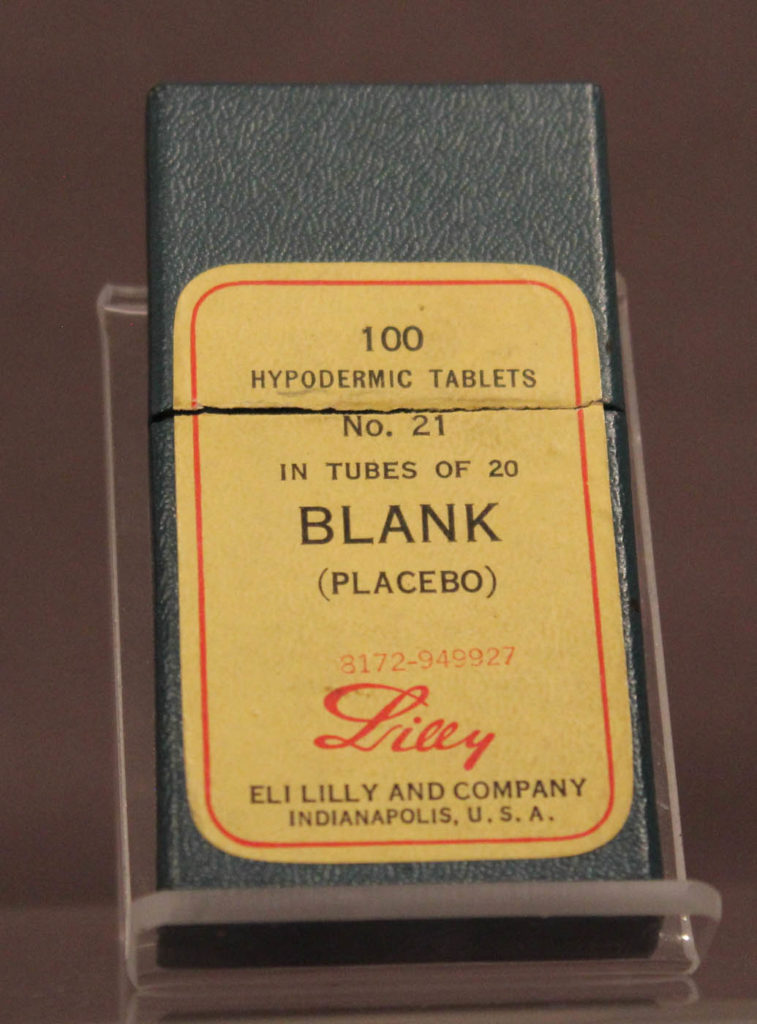
Scientists have come up with a new name for experiments that utilize placebos
Trick or treatment
+++++
I’m addicted to placebos.
I could quit but it wouldn’t matter.
+++++
On my way home from work today I was listening to Placebo..
I thought I was listening to something else, but obviously I was the control group.
+++++
Is that placebo working for you?
Well, now that you mention it, no.
+++++
My doctor is concerned my hypochondria is getting worse
So he put me on stronger placebos.
+++++
I got in trouble for using performance enhancing drugs
I took a placebo before my psychology exam
+++++
I was part of a scientific study on the calming effects of listening to the Three Tenors.
I felt great, but was in the control group. It turns out I was listening to Placebo Domingo.