Here’s an article from a blog called PRACTICAL ETHICS (Ethics in the News) at the University of Oxford. It’s pretty unfriendly to homeopathy, which we think isn’t quite as cut and dried a domain of practice as the author, Bennett Foddy, assumes. Brian, one of our founders, is happy to advise on both homeopathic and placebo regimes. That’s one point where we differ substantially with Foddy, and at least some of the literature does as well. Buying placebos from Boots, government subsidised or not, makes at least the ‘pleasing the practitioner’ script impossible. ("Pleasing the practitioner" is the idea that a patient’s trust in the authority of an expert induces the placebo effect.)
Tag Archives: Placebo Effect
What would convince you to use a placebo?

Here is an approach you may like to consider, to help you benefit from the mysterious healing powers of the placebo, even when you know it is a placebo you are taking; an approach that has been useful for a growing number of people in recent times, recommended by a homeopath of some 30 years experience.
Consider this . . . undoubtedly, there is a greater chance of success if the placebo taker believes it can work, and even more if the placebo taker trusts and has faith in the prescriber (which paradoxically can be themselves).
The simple mathematics around the mysterious healing powers of the placebo reveals an improvement in at least 30% (and up to 70%) of cases. You can be one of the 30-70%.
Our aim at universal Placebos is to help you shift from curiosity to action – to dare to try something new.
What would convince you to use a placebo? If you are curious you could try this simple procedure to evoke the positive qualities of Acceptance, Gratitude, Faith, Trust and Action.
Twice a day, say morning and night, take 3 placebo pilules.
With the first pilule focus on acceptance of who you are and where you are, all your advantages and disadvantages, strengths and weaknesses. Accept your true situation, so you are free to respond, and not just react.
As you take the second pilule focus on gratitude. Be thankful for all the positives you have in your life . . . “it could always be worse.” Be mindful of where you want to be. Have faith you will find inner guidance. . . just trust it, that these inner revelations are right and correct.
As you take the third pilule, just say YES . . . it feels better. Smile and go . . .take action with the first step, whatever that is . . . and believe it is possible.
Or, why not create your own ritual? Here are some tips:
(a) Apply KISS tactics (keep it simple sweetheart)
(b) Choose easy times to take placebos, like when you have a cuppa
(c) Take it at least twice a day, morning and night
(d) Be mindful and present in the moment
(e) Keep it short and easy to complete
The truth is that the successful outcome of any healing situation is determined by the actions and choices and healing system of the individual, regardless of the healing modality. Nobody can make anyone else better, but everyone needs some help sometimes.
The Placebo Effect on Fox: When You KNOW You’re Taking Placebo
 You know you’ve made it when they run a story on Fox News. Forget Harvard (where the groundbreaking placebo study took place that allowed patients to KNOW they were trialling placebos). The Harvard study told participants the ‘medication’ they were taking was inert, however it ‘would engage the mind-body and self healing thing’.
You know you’ve made it when they run a story on Fox News. Forget Harvard (where the groundbreaking placebo study took place that allowed patients to KNOW they were trialling placebos). The Harvard study told participants the ‘medication’ they were taking was inert, however it ‘would engage the mind-body and self healing thing’.
Marc Siegel, from something called the ‘Fox News Medical A-Team’, comments on video here.
In other news, the more mainstream Wall Street Journal comments on the research here and here.
No fooling: ‘Placebo effect’ real

A simple sugar pill may help treat a disease — even if patients know they’re getting fake medicine.
The finding, reported online Wednesday in the journal PloS One, may point the way to wider — and more ethical — applications of the well-known “placebo effect.”
“The conventional wisdom is you need to make a patient think they’re taking a drug, you have to use deception and lies,” said lead author Ted Kaptchuk, an associate professor of medicine at Harvard Medical School. And, Kaptchuk added, it seems many doctors do this: In one report, as many as half of rheumatologists and internists surveyed said they had intentionally given patients ineffective medication in the hopes it would have a positive result.
Kaptchuk, however, wondered whether the deception was needed. When he first tried to persuade fellow researchers to explore a sort of “honest” placebo, “they said it was nuts,” he said. After all, didn’t the whole effect hinge on people believing they were getting real treatment?
Patients were easier to enlist. “People said, ‘Wow, that’s weird’ and we said, ‘Yeah, we think it might work.'”
The researchers enrolled 80 people suffering from irritable bowel syndrome, explaining the experiment while framing it positively — they called it a novel “mind-body” therapy.
Half the patients were given a bottle with the word “placebo” printed on it. The pills it held, they were told, were like sugar pills. The patients were told they didn’t even need to believe in the placebo effect, but had to take the pills twice daily.
The other half were given no treatment at all.
At the end of the three-week trial, 59 percent of the patients taking the placebo said their symptoms had been adequately relieved, far outstripping the 35 percent in the non-treatment group.
“We were all taken aback,” Kaptchuk said. “We triple-checked the data before we decided it was real.”
Read the research paper at Plos One: Placebos without Deception: A Randomized Controlled Trial in Irritable Bowel Syndrome
“Placebo: Cracking the Code”
Featuring members of the the Harvard Placebo Study Group, “Placebo: Cracking the Code” examines the power of belief in alleviating pain, curing disease, and the healing of injuries. This is the first of several videos which can be accessed through Youtube – the first is below.
The placebo effect is a pervasive, albeit misunderstood, phenomenon in medicine. In the UK, over 60% of doctors surveyed said they had prescribed placebos in regular clinical practice. In a recent Times Magazine article, 96% of US physicians surveyed stated that they believe that placebo treatments have real therapeutic effects.
Work on the placebo effect received an intellectual boost when the Harvard Placebo Study Group was founded at the beginning of 2001. This group is part of the Mind-Brain-Behavior Initiative at Harvard University, and its main characteristic is the interdisciplinary approach to the placebo phenomenon. The group is made up of 8 members: Anne Harrington (Historian of Science at Harvard), Howard Fields (Neuroscientist at Univ. of California in San Francisco), Dan Moerman (Anthropologist at Univ. of Michigan), Nick Humphrey (Evolutionary Psychologist at London School of Economics), Dan Wegner (Psychologist at Harvard), Jamie Pennebaker (Psychologist at Univ. of Texas in Austin), Ginger Hoffman (Behavioral Geneticist at Harvard) and Fabrizio Benedetti (Neuroscientist at Univ. of Turin). The main objective of the group is two-fold: to devise new experiments that may shed light on the placebo phenomenon and to write papers in which the placebo effect is approached from different perspectives.
Cutting Edge Research on the Placebo Effect
We were fascinated to see a story on Australia’s ABC News about recent research into the placebo effect. Pain researcher Damien Finniss, from Sydney’s Royal North Shore Pain Management and Research Institute, has published a paper in The Lancet on the phenomenon of the placebo effect. The ABC story makes two points which in our view have not received sufficient attention, namely:
* that the placebo effect is engaged even when a patient is aware s/he is receiving placebo (the ‘no-blind test’); and
* that responsible practitioners consider the agency of placebo in the course of treatment.

Consistent with other researchers we’ve read, Finniss and his colleagues are concerned with ethical issues in practitioner-client relationships in consideration of conscious engagement with the placebo effect. This is what we’d expect from responsible researchers and health professional. At the same time, we’re aware of anecdotal evidence and some research (contained elsewhere in this blog) that in any case there is widespread ‘de facto’ use of placebos in general practice and elsewhere, as for example in the presciption of an antiobiotic in the treatment of a viral condition.
Placebo Discussions on Metafilter
Placebos – Wonder Drugs?
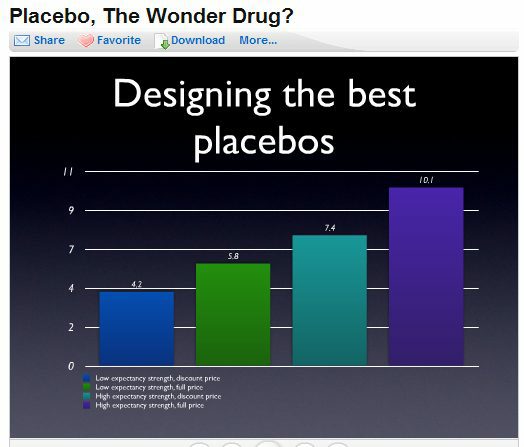
Here’s a web slide show with Mike Campbell and Alan Jones presenting on placebos at the Interesting South Conference, 20th August 2009. They even came up with a consent form allowing a doctor to prescribe placebos as needed …!
Placebos are getting under the skin of the drug pushers
It sounds counter-intuitive, but it seems that placebos are geting ‘stronger’ … or more to the point, the placebo effect is increasingly recognised as touching the heart of the overall process of healing and the nature of wellness. A fascinating article on this dynamic phenomenon in Wired magazine – looks like the debate is going mainstream!
And lest we forget … there’s money at stake. Big money.
Giving placebos could help patients?
According to this article from the ‘OnMedica’ medical website, doctors are being encouraged to consider the “meta-placebo” effect: ‘the healing belief that even fake/placebo treatments have positive effects . . . if both the doctor and the patient believe in the healing powers of the fake treatment, it does not matter that both know the treatment is fake’. No need to wait for medical tests to verify this hypothesis. A growing number have already experienced this effect using our Universal Placebos. See our Testimonials page.
Tuesday, 5 August 2008

Doctors could steer patients away from unproven alternative therapies if they could use dummy pills, suggests Dutch research.
Oskar van Deventer, a researcher from Leidschendam in the Netherlandspoints out that it is a well established medical fact that fake treatments do work.
If this is the case, he argues, doctors could include placebo pills in their medical armamentarium. But then the doctor might have to lie to the patient and this would present an ethical dilemma.
“On the one hand, the doctor does not want to lie to his patient. On the other hand, the effect of the fake treatment would diminish if the patient knows it is fake. For this reason, fake treatments are typically left to practitioners of so-called alternative medicine who are often not even aware of the ethical dilemma,” he writes in the journal Medical Hypotheses.
However he believes this is not the case as telling the truth about the dummy treatment would not stop it from being effective. This type of treatment is called the ‘meta-placebo’ effect.
“This is based on the healing belief that even fake/placebo treatments have positive effects. That is, if both the doctor and the patient believe in the healing powers of the fake treatment, it does not matter that both know the treatment is fake,” he says.
If such an effect does exist, it would solve a few complexities for today’s medics. They would not have to lie to patients when prescribing them placebos and by having such treatments at their disposal they could continue to regularly monitor patients’ symptoms whilst on the “treatment”. The doctor could also help to prevent people from using alternative medicine, which can be both expensive and risky to health.
The hypothesis that the “meta-placebo” effect exists needs to be tested before such treatments can become evidence-based medicine.
Using the equivalent to the gold standard of the double blind trial would create a challenge for such research as would the dilemma over which condition to test it on, he says, but he calls on readers to help meet those challenges in testing the effect.
The article follows figures published by the Prescription Pricing Authority last month that show a fall in the prescribing of homeopathic remedies by GPs from 83,000 in 2005 to 49,300 in 2007.
However separately, a pilot study from five NHS homeopathic hospitals found 60% of the 1797 patients treated with homeopathic remedies reported an improvement in quality of life.
The top four most treated conditions were eczema, chronic fatigue syndrome, menopause and osteoarthritis. Amongst those four, the proportion of patients that reported an improvement in quality of life after six visits to the homeopath varied from 59.3% for chronic fatigue syndrome and 73.3% for menopause. Overall, 30 common conditions were being treated by homeopaths.
Medical Hypotheses 2008; 71: 335–9; Homeopathy 2008; 97: 114-121