(Medical Xpress)—Imagine that your doctor knows from evidence-based studies that if he tells you about certain, small side-effects to a particular drug, you are significantly more likely to experience that side effect than if he did not tell you about it. Given the three values of autonomy, beneficence, and nonmaleficence, what should he do?
On the flip side, what if your doctor knew that statistically patients who are gradually weaned off of a chronic pain medication by decreasing their dosage until it is a placebo will still experience relief from their pain as a result of habituation? Should the doctor lie to you about your dosage in an effort to help your chronic pain while mitigating side effects?
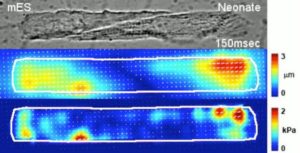
Mark Alfano, bioethicist at Delft University of Technology in the Netherlands writes a compelling argument for re-defining our views of placebos and placebo effects and how, by defining them in terms of classical conditioning, expectation fulfilment, and somatic attention and feedback, the ethics of informed consent changes by doing so. His is the target article in this month’s issue of the American Journal of Bioethics.
More information: “Placebo Effect and Informed Consent” American Journal of Bioethics, 15:10, 3-12.